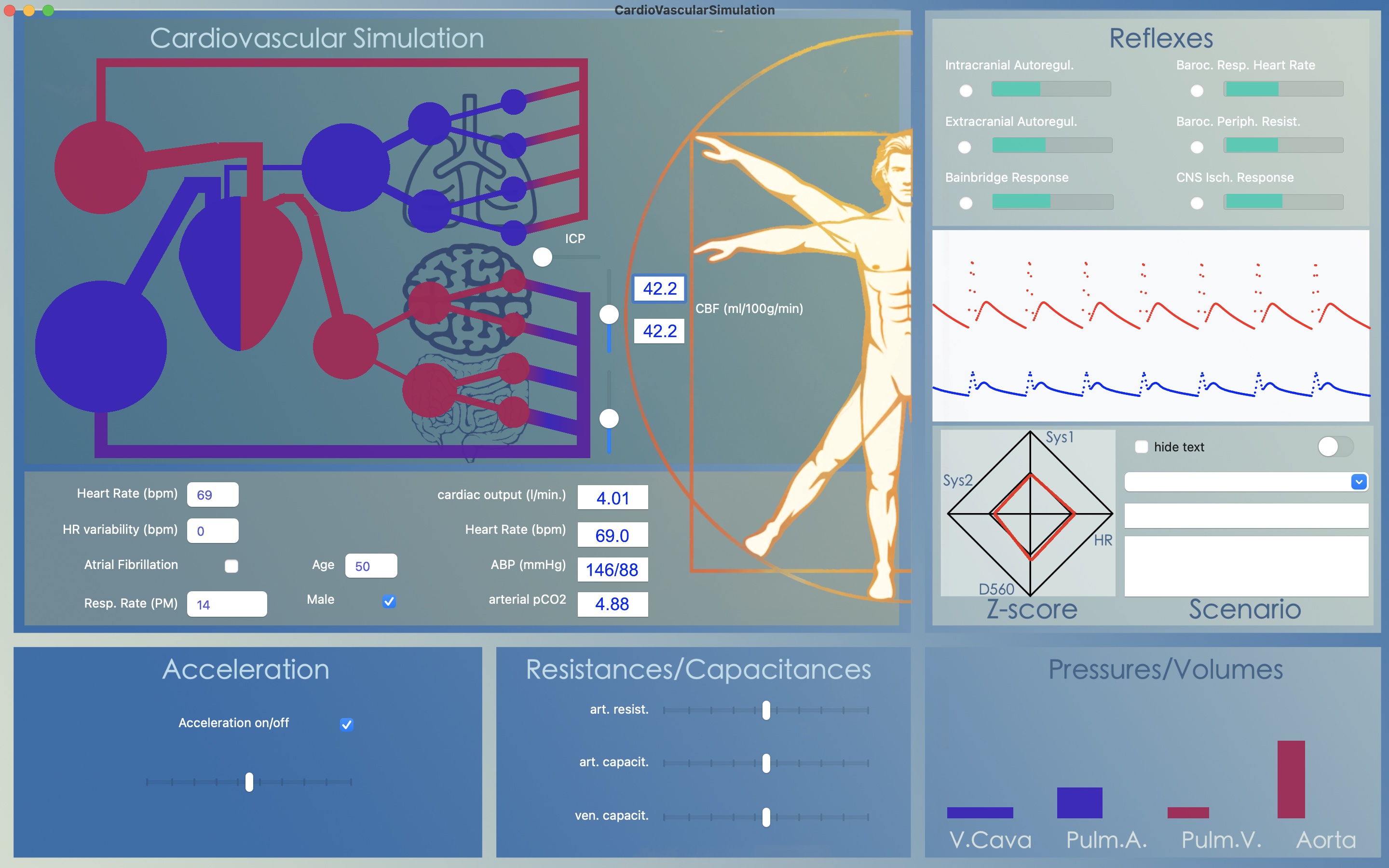
Developing the cardiovascular simulation app is a time consuming undertaking. With a working app: what are the goals achieved?
These are the most important inferences:
The heart is in essence a volume pump
Short term regulation of circulation combines humoral and mechanical mechanisms
Cardiac output depends on heart frequency and venous capacity
Venous capacitance is hypothetically governed by the CNS ischemic response
Cerebral autoregulation is the net result of the metabolic response and the CNS ischemic response
The most important achievement of the cardiovascular simulation app is to illustrate the complexity of the different regulatory mechanisms, humoral and mechanical. The model confines itself to only the mechanisms working in the short term. The model ignores all mechanisms ensuring adequate blood volume and blood content for the long term such as glucose regulation, regulation of electrolytes, regulation of pH, regulation of blood osmolality, etc. etc. Biological systems based upon hundreds of million years of evolution are layered systems that provide homeostasis in a highly complex and chaotic way, with their efficiency mainly based upon so many years of trial-and-error.
Evolution is based upon variation in large populations and a single individual is of little or no importance. It is a striking paradox how much Western communities invest in health care for the individual.
The following settings are automatically saved at app closure and retrieved at app re-activation:
parameter |
initial parameter value |
|
heart rate |
67 BPM |
|
heart rate variation |
0% |
|
respiratory rate |
14 PM |
|
age |
50 yrs |
|
sexe |
male |
|
atrial fibrillation on/off |
off |
|
acceleration on/off |
off |
|
acceleration factor slider |
half scale |
|
arterial resistance slider |
at indicator at 1/4th of full scale |
|
arterial capacitance slider |
at indicator at 1/4th of full scale |
|
venous capacitance slider |
at indicator at 1/4th of full scale |
|
ICP value slider |
0 mmHg |
|
brain CO2 consumption slider |
half scale |
|
body CO2 consumption slider |
half scale |
|
respiratory auto regulation on/off |
off |
|
arterial acceleration auto regulation on/off |
off |
|
tilt table angle slider |
0 deg. |
|
brain metabolic response on/off |
off |
|
body metabolic response on/off |
off |
|
Bainbridge response on/off |
off |
|
baroceptor to heart rate on/off |
off |
|
baroceptor to peripheral resistance on/off |
off |
|
CNS ischemic response on/off |
off |
|
maximum graph points |
80 |
|
heart sound (beep or heart rumors) |
off |
|
key strokes sound animation |
off |
|
S1 PaR or S2 PaR |
S1 PaR |
The following therapies are available
|
name |
effect |
time on (s) |
max at (s) |
time off (s) |
effect upon |
|
alteplase |
dissolves trombosis |
5 |
60 |
-- |
pulm.embol., car. occlusion, isch. stroke |
|
atropine |
increases heart rate with 70% |
0 |
30 |
180 |
all scenarios |
|
digoxine |
decreases heart rate with 40% |
0 |
90 |
300 |
all scenarios |
|
dopamine |
reduces venous capacitance with 30% |
0 |
60 |
-- |
all scenarios |
|
furosemide |
reduces blood volume with 500ml |
0 |
30 |
-- |
all scenarios |
|
heparin |
dissolves venous thrombosis |
5 |
60 |
-- |
cerebral and systemic venous thrombosis |
|
mannitol |
reduces ICP with 60% |
0 |
90 |
300 |
all scenarios |
|
metropolol |
reduces systemic arterial resistance with 60% |
0 |
120 |
300 |
all scenarios |
|
norepinephrine |
increases systemic arterial resistance with 100% |
0 |
30 |
-- |
all scenarios |
|
nitroglycerin |
increases venous capacitance with 40% | 0 | 120 | -- | all scenarios |
|
saline |
increases total blood volume with 250ml | 0 | 60 | -- | all scenarios |
Up to 6 therapies can be selected in total.
The following scenarios are available
|
name |
effect |
time on (s) |
time off (s) |
effect upon |
maximum amount |
| random scenario | select random scenario from list | ||||
| blood loss | reduce total blood volume | 0 | 300 | 2000ml | |
| sepsis | increase venous capacitance | 0 | 300 | venous | +50% |
| decrease arteriolar resistance | 0 | 300 | cerebral and systemic | -33% | |
| pulmonary embolism | increase arterial resistance | 0 | 300 | half of pulmonary arteries | *60 |
| right decompensation | reduce ejection fraction | 5 | 200 | right side of the heart | -30% |
| left decompensation | reduce ejection fraction | 5 | 200 | left side of the heart | -30% |
| venous thrombosis | increase venous outflow resistance | 0 | 600 | systemic venules outflow resistance | *3 |
| ICP elevation | step in- and decreases in ICP | 0 | 600 | venous outflow pressure | +50mmHg |
| ischemic stroke | increase arterial resistance | 5 | 600 | half of carotid arteries | *60 |
| respiratory failure | reduce CO2 elimination in lungs | 0 | 300 | CO2 proportion removed | -80% |
| atrial fibrillation | increase heart rate & | 5 | 200 | heart rate | 110 bpm |
| turn atrial fibrillation on | 5 | 200 | heart rate variability | 20% | |
| cerebral venous thrombosis | increase venous outflow resistance & | 0 | 300 | cerebral venules outflow resistance | *3 |
| increase ICP | 0 | 300 | venous outflow pressure | +30mmHg | |
| aorta dissection | increase arterial resistance | 0 | -- | aorta | *4 |
| carotid occlusion | increase arterial resistance | 20 | 300 | half of cerebral arteries | *100000 |
| hyperventilation | increase CO2 elimination in lungs | 0 | 120 | CO2 proportion removed | *3 |
| CO2 retention | decrease CO2 elimination in lungs | 0 | 120 | CO2 proportion removed | *0.2 |
| cardiac arrest | stop regular heart beat | 10 | 90 | heart rate | *0.0001 |
| Valsalva manoeuvre | temporary increase in thoracic pressure | 5 | 20 | adds pressure to Cap1.0 and prevents venous backflow to the heart | +30mmHg |
| Migraine attack | vasospasm in outflow (hypothetical) | 5 | 300 | single cerebral outflow branch (Res1.8) | *2.0 |
| no scenario |
Therapy menu

The therapy menu contains different choices for medication to be applied to the model. Up to 6 therapies can be started simultaneously. Each therapy has its own effect on the cardiovascular system.
View menu

In the view menu options are provided to increase or decrease the total number of data points in the running graph of blood pressure (red) and middle cerebral artery flow (blue).
The graph mode can be altered for comparison of flow in different branches of the arterial tree. In later versions a simultaneous display of flow velocity signals can be displayed over the different branches of the arterial tree from proximal to distal. Optionally, these can be superimposed (starting from version 1.11).
Extra bars can be displayed either animating the pressure within the various capacitances or the hydrostatic pressure which depends on the head up tilt selected.
For feedback on the model performance FPS can be displayed. FPS will deteriorate when multiple windows are opened. The model performs best at an FPS over 120.
Optionally, a color legend can be added to show the range of colors used for indicating the CO2 level within the model resistances and capacitances.
Window menu

The window menu allows to add extra windows allowing to study aspects of the model function.
The window test parameters displays parameter settings of the model. Either modifiable or unmodifiable parameters are displayed.
The window patient condition displays the clinical condition of a symbolic patient
From version 1.9 onward a window can be added with clinical interpretation based upon Z-scores. Not all combinations of Z-scores lead to a clinical diagnosis. Work on automatic interpretation is ongoing.
The patient monitor displays vital patient parameters on a symbolic ICU monitor.
The analysis graphs allow to follow different model parameters as a function of time. There are three options: cerebral auto regulation, CO2 reactivity and ICP graphs. There are scenario's that can be used to follow the model behavior in response to changes in blood pressure, in CO2 level or in ICP.
The waveform NMA window allows to study the arterial blood pressure and middle cerebral artery wave form in more detail. There are three options: both signals versus time, middle cerebral artery flow versus blood pressure and middle cerebral artery flow versus blood pressure after normalization of the two signals. In version 1.11 the option was added to superimpose the raw flow velocity signals over a period of 10s. that underly calculation of the average flow used for NMA.
The time chart window displays the results of the NMA analysis over time. A NMA analysis is performed over 10 s intervals updated every 5 s. There are three options: cerebral blood flow, a combined plot of arterial blood pressure, middle cerebral artery flow and pCO2 and the pulsatile apparent resistance (PaR) and pulsatility index (PI).
Extra menu

The extra menu allows to change several menu settings:
selecting anesthesia will decrease the intra- as well as extra cranial metabolic rate with 50%.
selecting add noise to waveform will exactly do as it says, allowing to study the effect of averaging on the NMA analysis
selecting toggle S1 PaR will shift between the calculation of the pulsatile apparent resistance based upon the S1 measurement or upon the S2 measurement.
selecting sound will provide audible sounds to the model using either beeps like from an ICU monitor or auscultation sounds like from listening to heart activity.
selecting tilt anticipation will allow changes in the venous capacitance starting directly with the first change in head up tilt, as if the subject anticipates the effects of a change of posture. Without tilt anticipation the cardiovascular responses will lag to changes in body posture.
selecting variable acceleration with HR will cause the strength of the arterial acceleration to increase with a lower heart rate or with a longer RR'-interval.
selecting left<>right shunt provides four options between none, intermediate or full shunting between the left and right cerebral circulation. This shunt is of interest when the carotid occlusion scenario is chosen.
selecting specials aims to change the settings of the cardiovascular reflexes so that the model becomes like a patient with orthostatic hypotension or like a patient with postural orthostatic tachycardia syndrome.
selecting CardioVascularSimulationHelp has not been implemented so far
Tests menu
![]()
in the test menu the thermodilution method can be selected allowing to calculate an estimate for cardiac output by injecting a small amount of tracer in the right atrium. The surface below the concentration curve recorded more distally in the vascular system is calculated in order to make an estimate for cardiac output.
In version 1.11 the option was added to choose a block pulse cardiac output, instead of the more physiological sinusoidal output wave normally modeled. Selecting a block pulse gives a better impression of the model's viscoelastic properties and how it can be changed by selecting different values for the capacitance and resistance sliders in the lower mid portion of the front window.
-
IAG

In 2007 Neuromon BV was supported by a grant from the Innovative Action Programme Groningen and the EU.
-
Eureka label

For it's innovative work and collaboration with international partners Neuromon B.V. received the Eureka! label from the EU
-
Collaboration
To the benefit of patients on the Intensive Care Neuromon B.V. has joined forces with Compumedics DWL.